Medicines Optimisation
The AHSN NENC Medicines Optimisation programme, which was first launched in 2013, aims to ensure patients get the best from their medicines to improve outcomes.
The AHSN NENC team engage with networks of local, regional and national Medicines Optimisation professionals including local primary care networks (PCNs), North East Senior Pharmacy Managers Network, NENC CCG Prescribing Forum, Northern Treatment Advisory Group and various advisory groups.
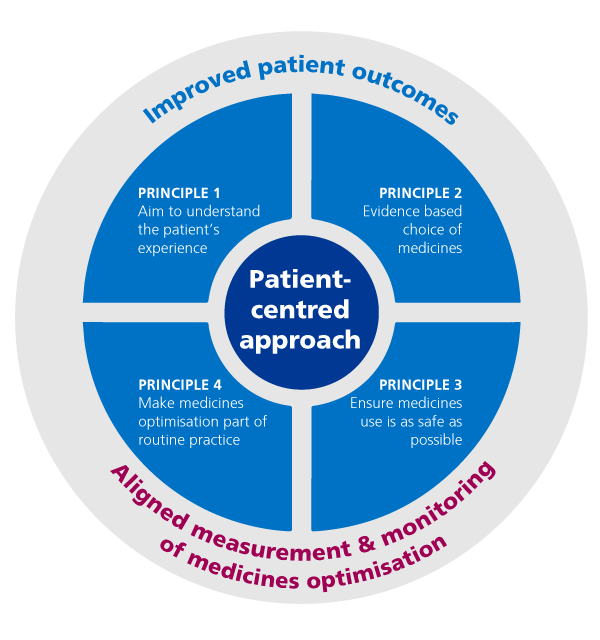
Image source: NHS England
The AHSN is currently engaged in supporting delivery of two national programmes, Polypharmacy: Getting the Balance Right, and the Medicines Safety Programme:
The Polypharmacy: Getting the Balance Right Programme aims to support local systems and primary care to identify patients at potential risk of harm and support better conversations about medicines by promoting shared decision making. One of the core principles of this is population health management.
The Medicines Safety Improvement Programme (MedSIP) aims to reduce severe avoidable medication related harm by 50% by March 2024 through medicines optimisation and quality improvement. There are two main focus areas in the programme; reduction in inappropriate high dose opiate prescriptions for non-cancer pain and safer administration of medicines in care homes.
Supporting Better Management of Chronic Pain in North East North Cumbria
Supporting primary care
To support Primary Care Network (PCN) pharmacy professionals the AHSN has collaborated with Health Education England to develop a PCN Community of Practice (CoP). If you are a pharmacist or pharmacy technician in the NENC and work in a GP practice then you can join our Future NHS Platform and access the CoP by completing this form:(https://www.smartsurvey.co.uk/s/NHSFuturePlatformRegistrationForm/).
Prescribing Data E-learning
NHS North of England Care Systems Support (NECS) have developed a prescribing data e-learning programme in conjunction with the AHSN NENC. It is available to any healthcare professional and will enable users to gain an understanding of how to access and use prescribing data.
Explainer video on the programme
Access Prescribing Data E learning
A prescribing data Elearning poster recently presented at the Clinical Pharmacy Congress in London. View the full poster zone.
Report – The Barriers and Opportunities for the Use of Digital Tools in Medicines Optimisation
In 2022, the AHSN NENC and NHS England Digital First Primary Care commissioned Newcastle University to produce a report on the barriers and opportunities for the use of digital tools in medicines optimisation across the interfaces of care. Following a three month period of research, the final report has been produced and can be downloaded here.
This report has also now been published by JMIR Publications view the report.
Events
Please view our events area for events related to this subject area. Past events will include presentations and recordings where available.
To find out more about the Medicines Optimisation programme please contact Helen Seymour, Medicines Optimisation Workstream Lead, [email protected]
Our Programmes
Reduce Opioid Prescribing
Opioids Opioids are a highly effective class of analgesics, and when used judiciously, are of great benefit to many people living with pain. However, in the case of ‘chronic non-cancer pain’, when the source of long-term pain does not have…
PolyPharmacy

HI NENC (formerly AHSN NENC) is supporting the delivery of a National Polypharmacy Programme: Getting the Balance Right in partnership with the NENC Integrated Care System (ICS), the national programme to support conversations about medicines between health professionals and the…
Electronic Repeat Dispensing (eRD)
This programme of work is now complete, please contact NHSBSA with any queries. The AHSN NENC is supporting a regional initiative coordinated by NHS England and Improvement Regional Office and The NHS Business Services Authority (NHSBSA) to increase the use…
PINCER
This programme of work is now complete, please contact [email protected] with any queries. PINCER is the Pharmacist-led Information technology iNtervention for the reduction of Clinically important ERrors in medicines management. The AHSN NENC is supporting PINCER in the region by…
Transfer of Care Around Medicines
This programme of work is now complete, please contact [email protected] with any queries. The AHSN NENC is aware that many trusts nationally are considering the use of the Transfer of Care Around Medicines (TCAM) project to support effective early discharge…
Medicines Adherence Support Project
This report is a summary of a 2-year investigation into the use of Multicompartment ComplianceAids (MCAs) in England. Within the report you will learn that hundreds of thousands of patients are inappropriately supplied these devices by pharmacies and pharmacists each…
Medicines Safety Improvement Programme
The Medicines Safety Improvement Programme (MedSIP) aims to reduce severe avoidable medication related harm by 50% by March 2024 through medicines optimisation and quality improvement. There are two main focus areas in the programme; reduction in inappropriate high dose opiate…